Our Services
How Hospice support works
Following a referral, we are able to see the patient and their family/whanau to assess what their immediate needs and concerns are. Referrals may come from a General Practitioner doctor (GP) or directly from the patient or their representative. To make a direct referral, please contact Clinical Manager Hannah Ledingham on 09 407 7799.
Our initial engagement can be a busy time ensuring that the approprite care is put in place, involving the patient, their family/whanau and the healthcare professionals. Our clinical team do not wear uniforms and our vehicles are unmarked, so we can visit you in confidence and maintain your privacy.
Our clinical team can be reached 24 hours a day by patients and their families to discuss their symptoms, medical care or to provide support if they become anxious or worried with questions and concerns.
Holistic Palliative Care
We provide palliative care when there is no curative option available. Our services are for people with any life-limiting illness, which may include heart failure, renal failure, cancer, motor neurone disease, emphysema or other illnesses. Our care is not limited to end-of-life and, with many patients and their whanau, a longer-term relationship can develop.
This includes management of our patient's pain and other symptoms, as well as engaging in conversations of honesty, truth and courageousness with patients and their family/whanau.
We work closely with our patients and their families/whanau to enable our patients to continue to live with meaning and purpose in their lives.
Support within Homes and Aged Residential Care
We support people to remain in their homes or their aged residential care, working closely with other health professionals to provide specialist advice, medical equipment, and support with a palliative approach to their care.

Medical Equipment
We own and loan specialist medical equipment to our patients free of charge, which can enable our patients to remain in their own home following our clinical assessment. It is our goal to support our patients to maintain their independence, and to stay safe and comfortable throughout their treatment.
Our equipment is commercially cleaned, delivered and installed in our patient's homes free of charge.


Hospice Mid-Northland Community Hospice on Assisted Dying
Three key points:
1. The intention of our service is to enhance the quality of life of patients and their loved ones, who are faced with the need for specialist palliative and end-of-life care, and to help them continue living every moment. A core philosophy of hospice is to neither hasten nor postpone death. This will not change.
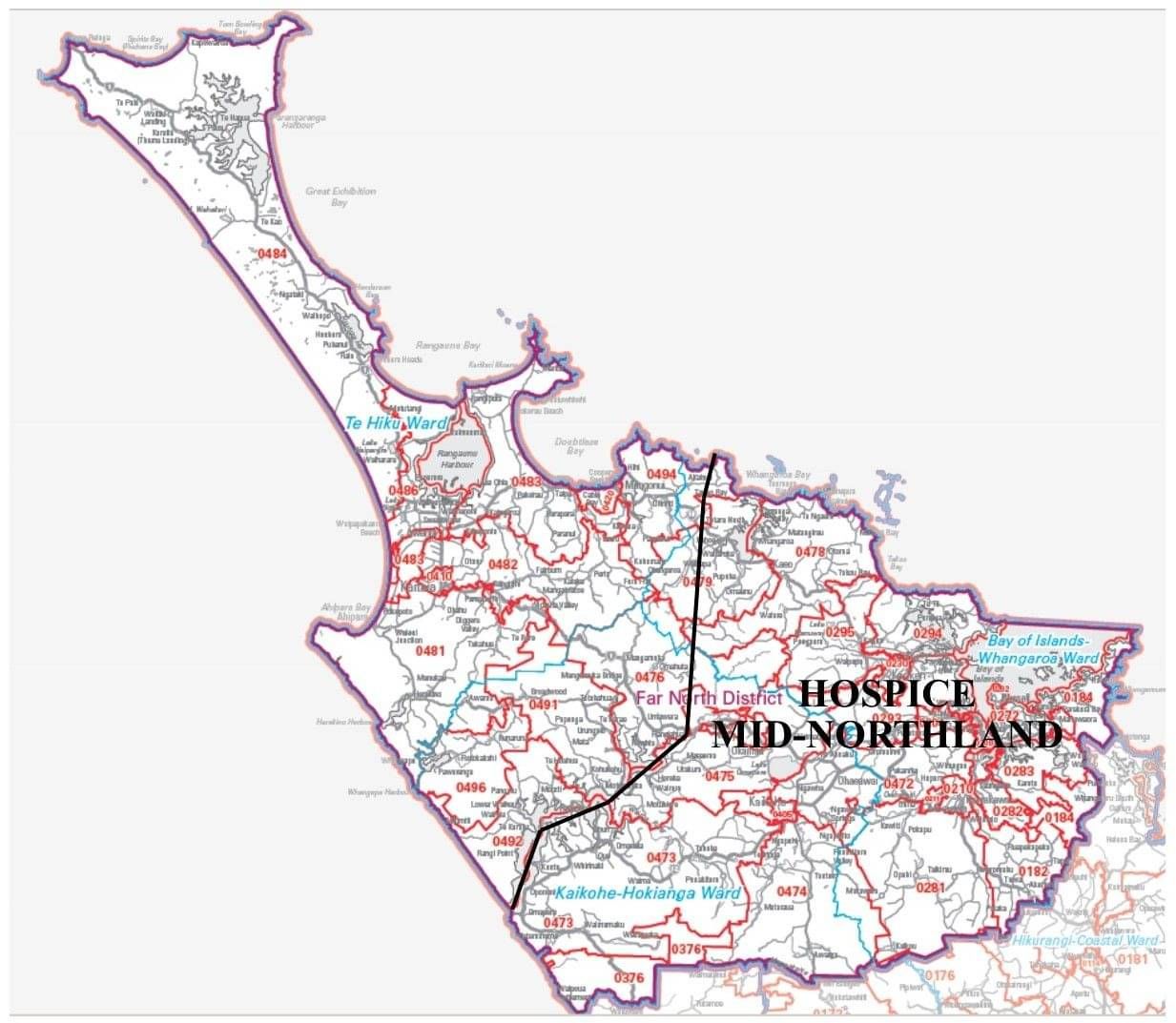
2. Our care will continue to be available, free of charge, to anyone with a terminal illness or life-limiting condition, who lives in our service area, including support for their families/whānau; regardless of their views on assisted dying (euthanasia or physician assisted suicide).
3. Hospice Mid-Northland staff and volunteers will not administer or be present for assisted dying procedures, nor can these procedures take place in the In-Patient Unit (IPU) in Whangarei or anywhere else on Hospice premises.
Hospice Mid-Northland Community Hospice are life-affirming services
Hospice Mid-Northland Community Hospice respects a person’s right to make choices, particularly around the end of their life.
We will continue to provide specialist palliative care and end-of-life care to any person needing support, regardless of their personal views on assisted dying.
However, Hospice Mid-Northland Community Hospice are not required to provide assisted dying procedures and have chosen not to do so. If we are aware of a patient’s request for assisted dying, we will continue to provide our care, as normal, until a non-hospice medical practitioner or nurse practitioner arrives at the patient’s home to carry out the procedure to end their life, OR the patient is transferred out of the IPU in Whangarei to their home or other place of choice for euthanasia or physician assisted dying.
Hospice care also continues for families/whānau during their bereavement. This important part of our service will not change, even if their loved one has opted for assisted dying.